-
The ovarian cycle is a series of changes that the ovaries undergo. The purpose of the ovarian cycle is the release of an oocyte ready for fertilization.
-
The menstrual cycle, also called uterine cycle, is a series of changes that the uterus undergoes. The purpose of the menstrual cycle is to prepare the uterus for the implantation of an embryo.
The ovarian and menstrual cycles are distinct but related. The cycles occur at the same time. The first day of the ovarian cycle corresponds to the first day of the menstrual cycle.
On average, the ovarian and menstrual cycles last 28 days, but they can range from 20 to 40 days.
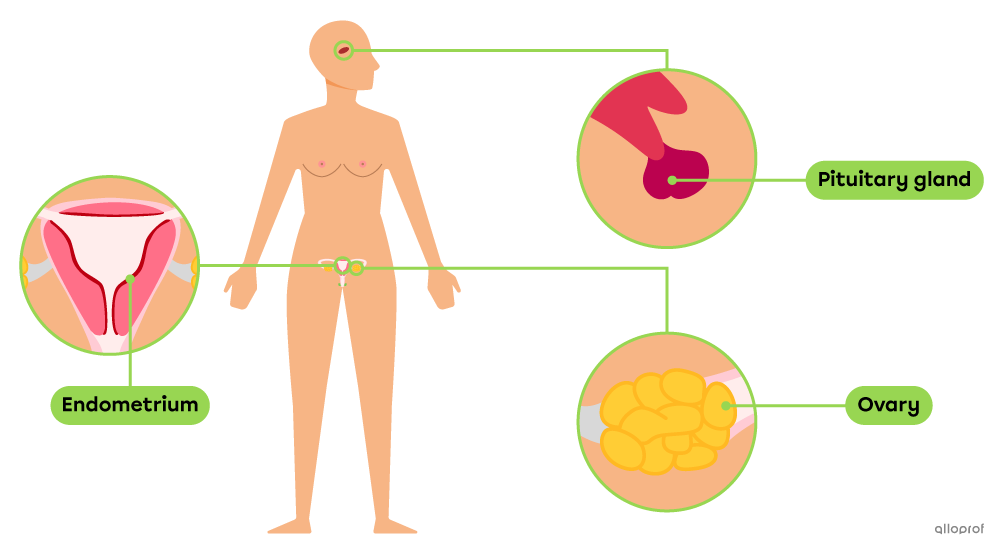
The pituitary gland, ovaries, ovarian follicle, oocyte, corpus luteum and endometrium are involved in the ovarian and/or menstrual cycles.
| Structures | Description |
|---|---|
| Pituitary gland | The pituitary gland is a small gland located at the base of the brain. It secretes several hormones including the follicle-stimulating hormone (FSH) and the luteinizing hormone (LH). |
| Ovaries | Ovaries are the glands of the female reproductive system. The steps of the ovarian cycle usually take place in one ovary at a time. |
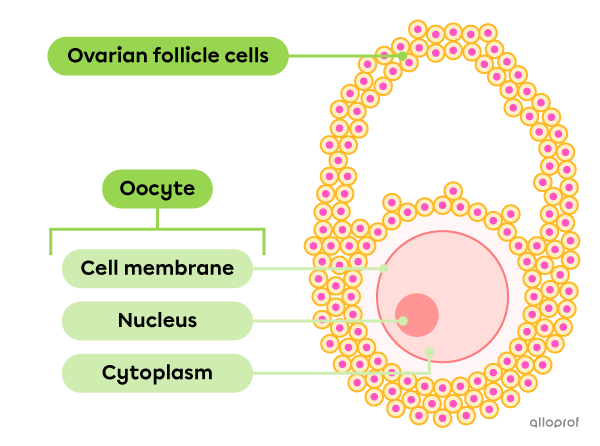
| Oocyte | An oocyte is an immature female gamete. It is one of the stages in ovum development. |
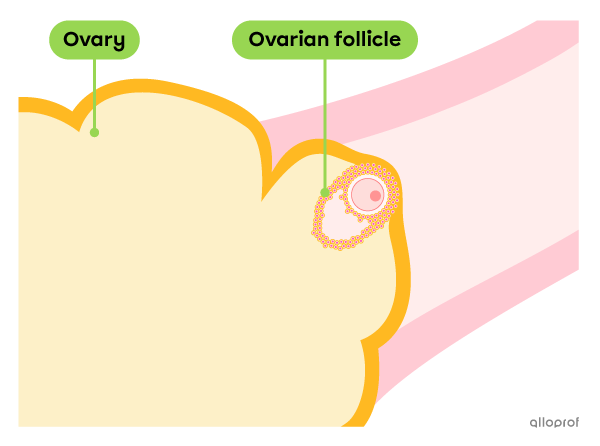
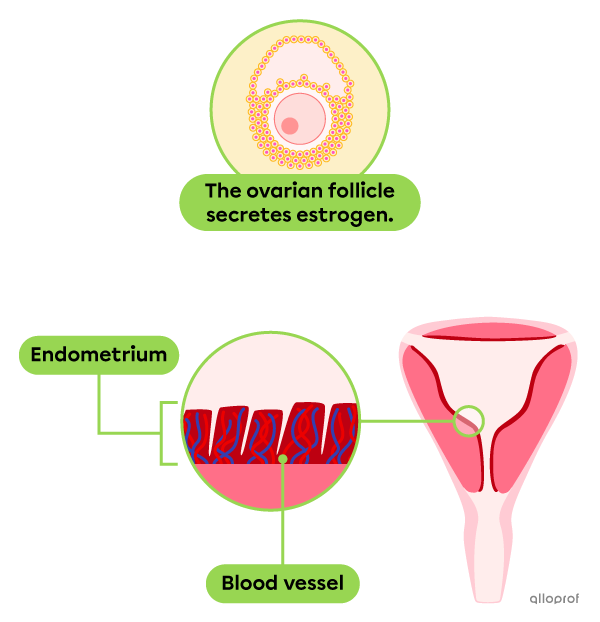
| Ovarian follicle | The ovarian follicle is a cell mass that protects and nourishes the oocyte. As it grows in the ovary, the ovarian follicle secretes estrogen. |
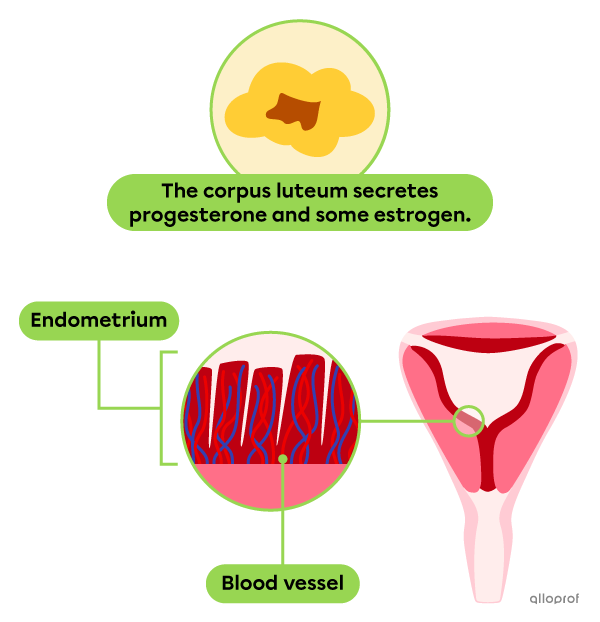
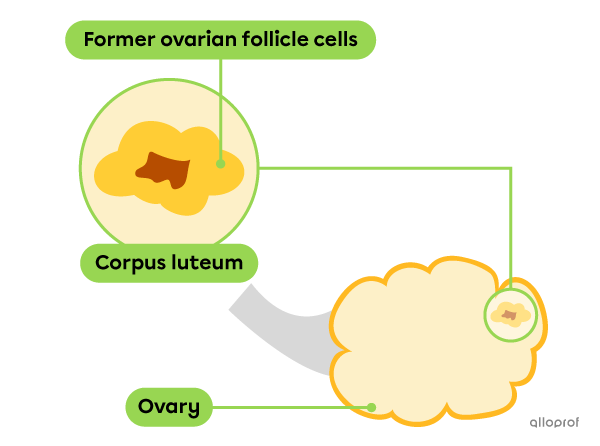
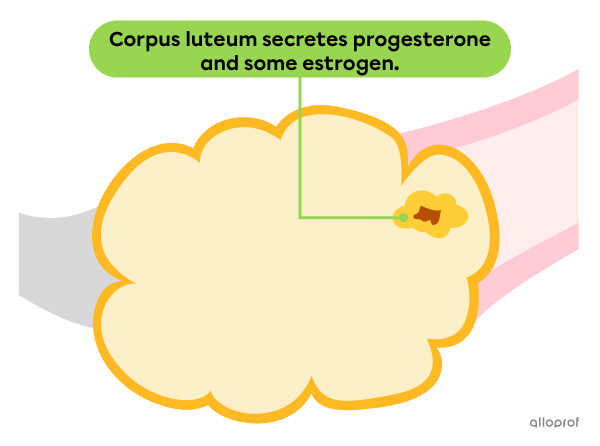
| Corpus luteum | The corpus luteum (pl. corpora lutea) is a small gland that forms from the cells of the ruptured ovarian follicle after ovulation. The corpus luteum is located in the ovary and secretes progesterone and some estrogen. |
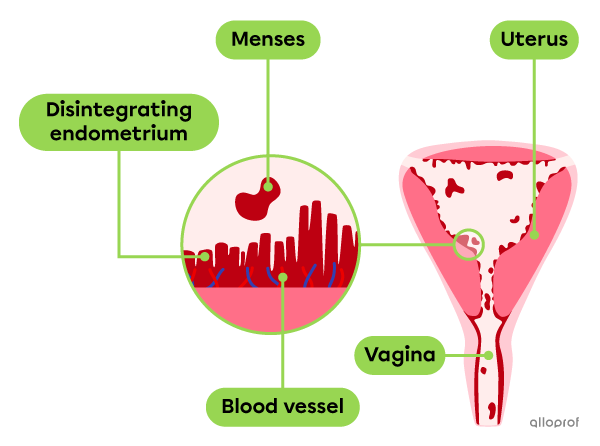
| Endometrium | The endometrium is a tissue rich in blood vessels. It covers the inner lining of the uterus. If fertilization occurs, this is where the embryo implants. |
The processes of the ovarian and menstrual cycles are caused by the action of FSH, LH, estrogen and progesterone.
-
The follicle-stimulating hormone (FSH) enables the growth of the ovarian follicle.
-
The luteinizing hormone (LH) enables the growth of the ovarian follicle, ovulation and healing of the corpus luteum.
-
Estrogen enables the regulation of FSH and LH.
-
Estrogen and progesterone enable the thickening and preservation of the endometrium.
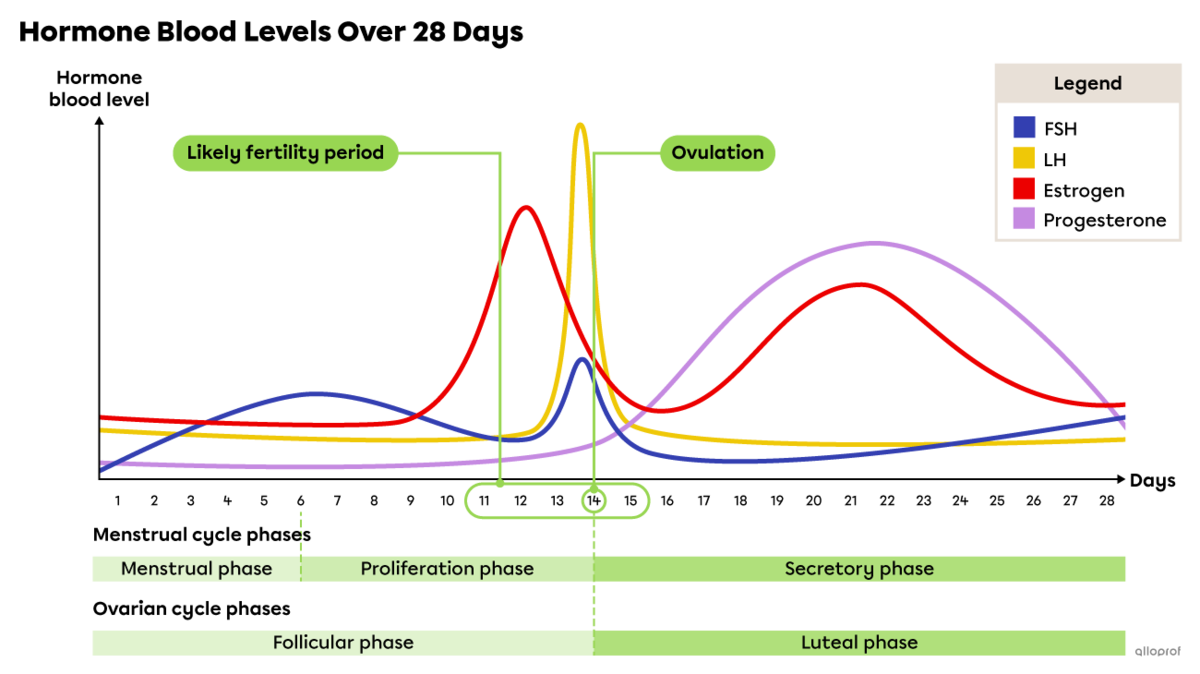
Based on a 28-day cycle, the highest level of FSH and LH is around day 14. The level of estrogen first peaks at the end of the follicular phase (proliferation phase of the menstrual cycle) and again during the luteal phase (secretory phase of the menstrual cycle). The level of progesterone peaks during the luteal phase (secretory phase of the menstrual cycle).
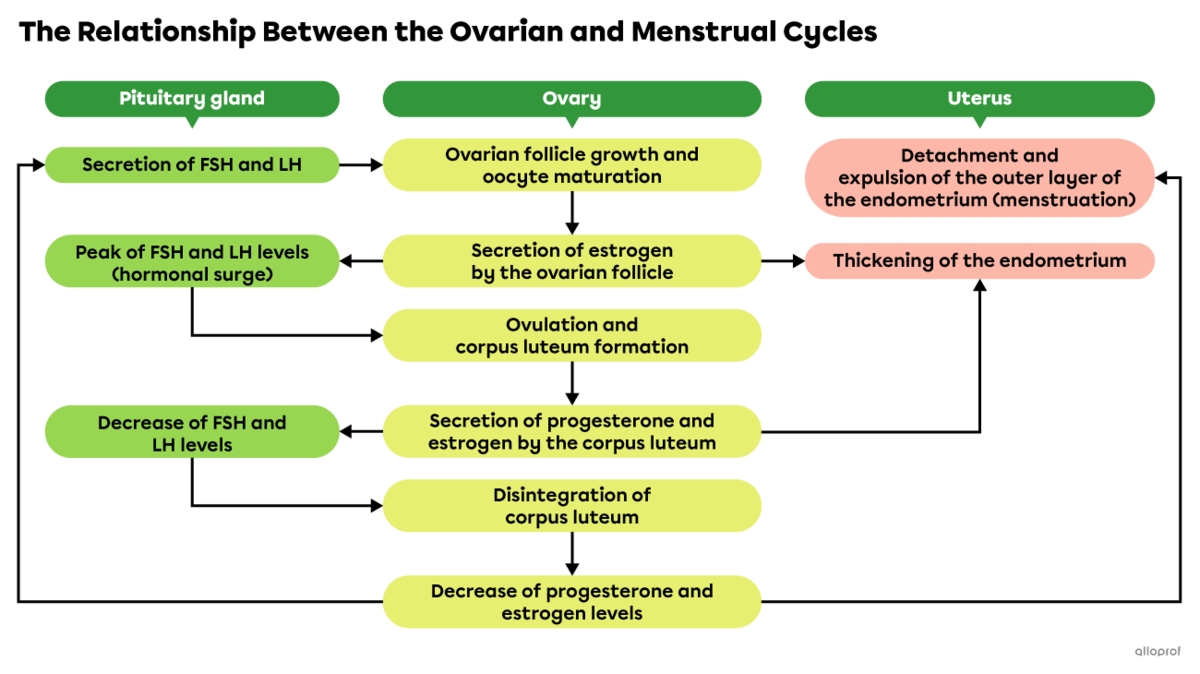
The following concept map relates the ovarian cycle to the menstrual cycle. It outlines the main changes in the pituitary gland, one of the two ovaries and the uterus.
During the ovarian cycle, one of the two ovaries undergoes several changes. First, an ovarian follicle grows and an oocyte matures inside it. When it is ready, the ovarian follicle ruptures and the mature oocyte is released towards the fallopian tube. Eventually, the remaining ovarian follicle becomes the corpus luteum. If the egg is not fertilized, the corpus luteum disintegrates and a new cycle begins. However, if the oocyte is fertilized, pregnancy begins. In this case, the corpus luteum remains for a few weeks.
The ovarian cycle consists of two phases: the follicular phase before ovulation and luteal phase after ovulation.
Based on a 28-day ovarian cycle, the follicular phase, also known as the preovulatory phase, generally corresponds to days 1 to 14.
During the follicular phase, the pituitary gland secretes FSH and LH to stimulate the growth of the ovarian follicle and the maturation of an oocyte.
As the ovarian follicle grows, it secretes more and more estrogen.

The increase in estrogen levels leads to a temporary decrease in FSH and LH levels.
By the end of the follicular phase, the ovarian follicle forms a bump on the surface of the ovary.
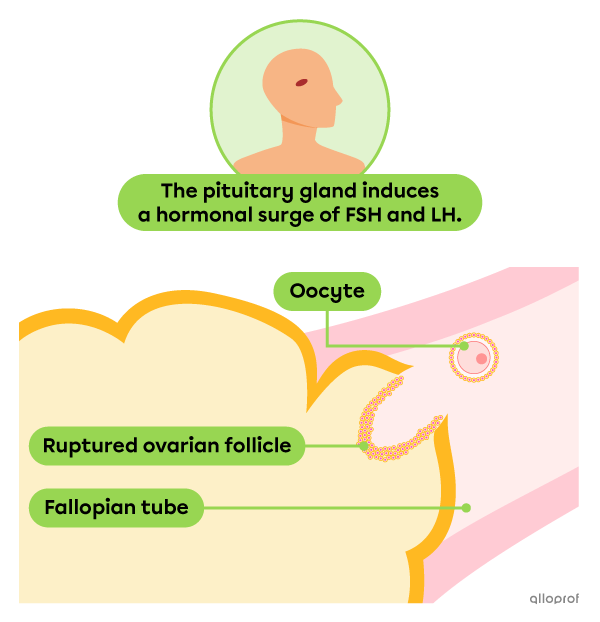
Ovulation is the release of a mature oocyte from the ovary towards the fallopian tube.
Based on a 28-day ovarian cycle, ovulation usually occurs around day 14.
When estrogen levels reach a certain point, FSH and LH levels peak: they rise drastically and then suddenly drop. This is called the hormonal surge. This rapid hormonal change strains the ovarian follicle, eventually causing it to rupture and release the oocyte towards the fallopian tube.
The fertility period refers to the days in the cycle when successful fertilization of an oocyte by a spermatozoon is most likely. This period depends on the lifespan of the spermatozoon released into the female reproductive system, as well as the lifespan of the oocyte released towards the fallopian tube. The fertility period lasts approximately 5 days.
-
Since spermatozoa can survive for about 72 hours (sometimes up to 120 hours), the fertility period starts approximately 3 days before ovulation.
-
Since the oocyte can survive for about 24 hours, the fertility period ends approximately 1 day after ovulation.
The following table describes the likely fertility period based on the duration of the ovarian cycle.
| Cycle duration | Ovulation day | Likely fertility period |
|---|---|---|
| 21 days | Day 7 | Days 4 to 8 |
| 28 days | Day 14 | Days 11 to 15 |
| 35 days | Day 21 | Days 18 to 22 |
The fertility period varies greatly from person to person and from cycle to cycle. Tracking cycles and fertility periods should not be used as the sole method of contraception.
Based on a 28-day ovarian cycle, the luteal phase, also known as the postovulatory phase, generally corresponds to days 15 to 28.
During the luteal phase, the cells of the ruptured ovarian follicle form a small gland, called corpus luteum. The corpus luteum secretes progesterone, a key hormone of the menstrual cycle, and some estrogen.
During this phase, the very low levels of FSH and LH prevent the growth of other ovarian follicles.
Corpus luteum only remains in the ovary temporarily. If the oocyte released during ovulation is not fertilized, the corpus luteum disintegrates after approximately 10 days due to the very low FSH and LH levels.
However, if the oocyte is fertilized, the corpus luteum remains active during the first weeks of the pregnancy.
During the menstrual cycle, the uterus undergoes a number of changes. First, the outer layer of the endometrium breaks down and flows out through the vagina. Then, the endometrium rebuilds itself by thickening more and more. By the end of the menstrual cycle, the endometrium is thick and full of blood vessels that supply it with blood and nutrients. It is ready to receive an embryo.
The menstrual cycle consists of three phases.
Based on a 28-day menstrual cycle, the menstrual phase usually corresponds to days 1 to 5.
During the menstrual phase, estrogen and progesterone levels are at their lowest. This leads to the breakdown of the surface layer of the endometrium. This layer contains, among other things, epithelial tissue, blood vessels and blood. This is called menses.
The muscle contractions force the menses out of the uterus. They leave the body by flowing out through the vagina.
Based on a 28-day menstrual cycle, the proliferation phase generally corresponds to days 6 to 14.
During the proliferation phase, the endometrium is rebuilt under the effects of estrogen secreted by the growing ovarian follicle. The endometrium thickens and new blood vessels form.
Based on a 28-day menstrual cycle, the secretory phase generally corresponds to days 15 to 28.
During the secretory phase, the endometrium prepares to receive an embryo. Under the effects of the progesterone secreted by the corpus luteum, the endometrium produces a fluid rich in nutrients for the potential embryo.
When fertilization does not occur, the very low LH level leads to the loss of the corpus luteum and simultaneous decrease in estrogen and progesterone levels. The thickening of the endometrium stops. The blood vessels of the endometrium contract and stop supplying it with nutrients and oxygen |(\text{O}_2).| This marks the end of this menstrual cycle and the beginning of a new cycle (return to the menstrual phase).